
Dr. Dale Avers is a Professor in the Physical Therapy Education Program at Upstate Medical University. She is internationally recognized as one of the foremost authorities on exercise programs designed to help older adults maintain or improve function and, perhaps most importantly, prevent falls.
The statistics on falling are of great concern. According to the Centers for Disease Control and Prevention (CDC) and other authorities:
- Between 25-33% of adults 65 years and older suffer a fall each year.
- Falls are the number one cause of injury in this population,
- 3 million people are treated in emergency rooms and 800,000 people are hospitalized each year for treatment of injuries that are the result of falls, with medical costs in 2015 totaling over $50 billion.
- Globally, falls are the second leading cause of unintentional injury death.
The causes of falls are numerous and can include the effects of disease, such as poor sensation in the feet due to diabetes; effects of medications; inner ear problems causing poor balance; or vision deficits, to name just a few. But according to Dr. Avers, perhaps the most easily-changed cause of increased falls is the loss of muscle strength so consistently seen in older adults, which is due in large part to inactivity and, yes, just the general decline seen with advancing years. The rate of that decline, however, can be lessened very significantly if one exercises consistently.
Now, you may be thinking right now – I’m a runner; I exercise vigorously 30-60 minutes, 5 days a week. Isn’t this a deposit in my fall-prevention account? Well, the answer is, Yes – to a certain degree, but maybe not enough. Dr. Avers will tell you that running, and other aerobic exercise routines such as swimming or biking, primarily improve your longevity odds by increasing your cardiovascular fitness, but it is a strengthening program – aggressive, resistance exercise – that improves function and most effectively reduces the incidence of falls.
To be effective, a strengthening program must be challenging. Lifting a two-pound weight 50 times is not going to produce the gains in strength required to maximize function. A weight you can lift just 8-12 times, one set, twice weekly for a particular muscle group (e.g., squats or calf raises) is more in line with what will truly make a difference. Strengthening, coupled with general balance exercises such as single-leg stance, is what has over the past decade or so been prescribed by physical therapists and others to help older adults minimize their fall risk.
More recent research, however, has shown that while this approach will result in improvements, it may not be truly optimal. Dr. Avers makes a strong case for the addition of exercises that improve power as well as strength, and drills that help train individuals to recover their balance when their equilibrium is upset by being jostled unexpectedly or tripping over something. What is needed are quick, explosive (ballistic) movements such as jumping, hopping, or side-to-side running or cutting routines that will help to develop quick reaction time (what many people erroneously refer to as “reflexes”). Again, these do not need to be done daily; 2-3 times per week should suffice.
Below are some suggested exercises Dr. Avers recommends all individuals – of any age, but especially those over 60 – add to their routine. The good news is that in addition to improving your fall risk odds, these exercises are likely to help you improve your running speed by increasing your muscle power.
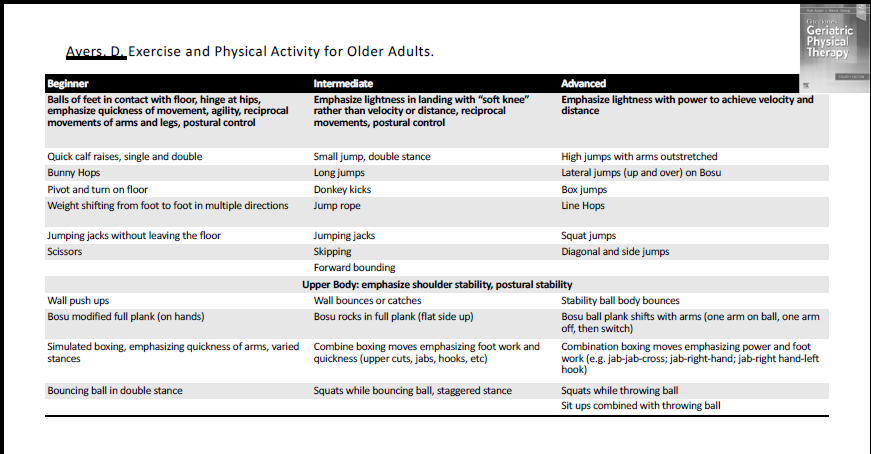
| Avers, D. Exercise and Physical Activity for Older Adults. 4th Edition. Ed: Avers, D. & Wong, R. Guccione’s Geriatric Physical Therapy. 4th edition. Elsevier, St. Louis. 2020 pg 185. |
